EFFECT OF A BACKBOARD ON
CHEST COMPRESSION QUALITY
DURING IN-HOSPITAL
CARDIOPULMONARY
RESUSCITATION
A RANDOMISED
,
SINGLE-
BLINDED,
SIMULATION SUPERIORITY TRIALAantal woorden: 6078
Zara Cuvelier
Stamnummer: 01809452
Ruben Houthoofdt
Stamnummer: 01305065
Promotor: Prof. dr. Stijn Blot Copromotor: Drs. Brecht Serraes Copromotor: Dr. Nicolas Mpotos Mentor: Dhr. Carl Haentjens
Masterproef voorgelegd voor het behalen van de graad van master in de verpleegkunde en de vroedkunde
©Copyright UGent
Without written permission of the thesis supervisor and the authors it is forbidden to reproduce or adapt in any form or by any means any part of this publication. Requests for obtaining the right to reproduce or utilize parts of this publication should be addressed to the promotor.
A written permission of the thesis supervisor is also required to use the methods, products and results described in this work for publication or commercial use and for submitting this publication in scientific contests.
EFFECT OF A BACKBOARD ON
CHEST COMPRESSION QUALITY
DURING IN-HOSPITAL
CARDIOPULMONARY
RESUSCITATION
A RANDOMISED
,
SINGLE-
BLINDED,
SIMULATION SUPERIORITY TRIALAantal woorden: 6078
Zara Cuvelier
Stamnummer: 01809452
Ruben Houthoofdt
Stamnummer: 01305065
Promotor: Prof. dr. Stijn Blot Copromotor: Drs. Brecht Serraes Copromotor: Dr. Nicolas Mpotos Mentor: Dhr. Carl Haentjens
Masterproef voorgelegd voor het behalen van de graad van master in de verpleegkunde en de vroedkunde
This page is not available because it contains personal information.
Ghent University, Library, 2021.
This page is not available because it contains personal information.
Ghent University, Library, 2021.
Table of content
1 Preface ... 6 2 Argumentation duo-thesis ... 7 3 Abbreviations ... 8 4 Abstract ... 9 4.1 English abstract ... 9 4.2 Dutch abstract ... 10 5 Introduction ... 11 6 Methods ... 14 6.1 Study design ... 146.2 Setting and sample... 14
6.3 Intervention ... 14
6.3.1 Phase one ... 15
6.3.2 Randomisation ... 16
6.3.3 Phase two ... 16
6.4 Outcome measures and covariates ... 19
6.5 Sample size calculation ... 19
6.6 Statistical methods ... 20
6.7 Ethical considerations ... 20
7 Results ... 21
7.1 Effect of a backboard ... 23
7.2 Influence of age, sex, BMI and department ... 27
8 Discussion ... 29
8.1 Effect of a backboard ... 29
8.2 Influence of age, sex, BMI and department ... 35
5
8.4 Study limitations ... 38
9 Conclusion ... 40
10 References ... 41
11 Appendix ... 50
11.1 Appendix 1: Recruitment flyer ... 50
11.2 Appendix 2: Feedback and feedforward CPRTEST® software (Pinga Group, Belgium) ... 51
11.3 Appendix 3: Participant information letter and written informed consent ……….…………52
6
1
Preface
“The most challenging times bring us the most empowering lessons” - Karen Salmansohn.
This thesis marks the conclusion of our master’s degree in nursing at Ghent University. Challenging might be an understatement, but we are deeply grateful for both the personal and professional growth and enrichment that came along with it. Therefore, we would like to sincerely thank some people who were indispensable during this process.
Firstly, we would like to thank our supervisor Prof. dr. Stijn Blot for his support, guidance and critical but constructive feedback. We would also like to show our gratitude to our co-supervisors for their commitment, valuable feedback, critical minds and encouraging words. Their strive for quality lifted our work to a higher level. We also thank them for their technical and logistical support before and during the data collection process. Furthermore, we want to thank our mentor for putting some CPR training in the hospital on hold in order to increase the number of participants training CPR within our study.
Secondly, we would like to thank all participants for their participation as well as all head nurses, volunteers and the ICT department of the hospital for facilitating and assisting during data collection in this study. We would not have been able to conduct this research without them.
Furthermore, a sincere thank you goes out to our boyfriend/girlfriend, friends and family for their continuous support, love and belief in our abilities.
Finally, we want to express our gratitude to our parents for the unconditional love and unmatched support during this challenging process. We are beyond grateful for the opportunity that they provided for us to broaden our training as professional emergency nurses at Ghent University.
7
2
Argumentation duo-thesis
This study included a labor-intensive data collection process with active observation of the participants at all times. We insisted on an approachable participation in the study for our participants, resulting in extensive opening hours of the study room, multiple days a week during a series of fifteen weeks. We believed that flexibility was the key to recruit nurses, dealing with heavy workload on the ward. Since a relatively large sample size was required in order to obtain statistically significant results, assigning only one researcher to this study would result in either a prolonged data collection with higher dropout risk or a smaller sample size. This duo-master thesis enabled us to recruit a larger sample within the limited time frame of a thesis and thus provided the opportunity to develop stronger evidence on the research subject. In addition, a more extensive sample size also provided the opportunity for more extensive statistical analyses (sub-analyses) and therefore broadened our research objective resulting in multiple study aims.
Description of responsibilities within the thesis:
- Both students: creating study design, searching and reviewing relevant literature, recruiting participants, carrying out data collection, conducting data analysis and verifying/adding to each other’s written thesis sections.
- Ruben Houthoofdt: writing the introduction, results and discussion (impact of sex, department, BMI and age) and designing recruitment flyer.
- Zara Cuvelier: writing the abstract, methods, discussion (effect backboard, limitations and recommendations for clinical practice and further research), conclusion and designing participant flow chart.
8
3
Abbreviations
BLS Basic life support BMI Body mass index BPM Beats per minute CC Chest compressions CI Confidence interval
CPR Cardiopulmonary resuscitation C:V ratio Compression-to-ventilation ratio ERC European Resuscitation Council IHCA In-hospital cardiac arrest
ILCOR International Liaison Committee on Resuscitation IQR Interquartile range
RCT Randomised controlled trial
9
4
Abstract
4.1 English abstract
Introduction: According to the European Resuscitation Council, chest
compression quality during in-hospital resuscitation is often suboptimal on a soft surface. Scientific evidence regarding the effectiveness of a backboard is lacking and equivocal. This single-blinded manikin study evaluated the effect of a backboard on compression depth, rate and chest recoil. Sex, BMI, age and department were considered as potential predictors.
Methods: Using self-learning, a consecutive sample of 278 nurses was retrained
to achieve a combined compression score of ≥70%, consisting of ≥70% compressions with depth 50-60mm and ≥70% compressions with complete release (≤5mm) and a mean compression rate of 100-120bpm. Nurses were allocated to a backboard group and control group and performed a two-minute cardiopulmonary resuscitation test in bed. The main outcome measure was the difference in proportion of participants achieving a combined compression score of ≥70%.
Results: In total, 158 nurses dropped out and 120 were allocated to a backboard
group (n=61) and a control group (n=59) with equal baseline characteristics. The proportion of participants achieving a combined compression score of ≥70% was not statistically significantly different (p= 0.475) and suboptimal in both groups: backboard group 47.5% and control group 41.0%. Specifically the age category ≥51 years was a significant predictor for a combined compression score of ≥70% [OR = 0.133; 95% confidence interval (CI), 0.037-0.479; p=0.002].
Conclusion: This simulation study indicated that chest compression skills were
important in both groups. Using a backboard did not significantly improve compression quality. Well-designed studies must be conducted to confirm these findings.
10 4.2 Dutch abstract
Inleiding: Volgens de Europese reanimatieraad is de borstcompressiekwaliteit
vaak suboptimaal tijdens een intrahospitale reanimatie op een zachte ondergrond. Wetenschappelijke bewijskracht voor de effectiviteit van een reanimatieplank ontbreekt en is tegenstrijdig. Deze geblindeerde oefenpopstudie evalueerde het effect van een reanimatieplank op de compressiediepte, -frequentie en terugvering van de thorax. Geslacht, BMI, leeftijd en dienst werden beschouwd als potentiële predictoren.
Methode: Via een zelfleerstation werd een consecutieve steekproef van 278
verpleegkundigen bijgeschoold tot een gecombineerde compressiescore van ≥70%, bestaande uit ≥70% compressies met diepte 50-60 mm en ≥70% compressies met volledige loslating van de thorax (≤5 mm) en een gemiddelde compressiefrequentie van 100-120 per minuut. Participanten werden toegewezen aan een groep met en zonder reanimatieplank en voerden een reanimatietest van twee minuten uit in bed. De primaire uitkomstmaat betrof het verschil in proportie deelnemers met een gecombineerde compressiescore van ≥70%.
Resultaten: In totaal vielen 158 verpleegkundigen af en werden er 120
toegewezen aan een interventiegroep (n=61) en controlegroep (n=59) met gelijke demografische karakteristieken. De proportie deelnemers met een gecombineerde compressiescore van ≥70%, was statistisch niet significant verschillend (p = 0.475) en suboptimaal in beide groepen: met (47.5%) en zonder reanimatieplank (41.0%). De leeftijdscategorie ≥51 jaar was een significante voorspeller voor een gecombineerde compressiescore van ≥70% [OR = 0.133; 95% betrouwbaarheidsinterval, 0.037-0.479; p = 0.002].
Conclusie: Deze simulatiestudie demonstreert dat borstcompressievaardigheden belangrijk waren in beide groepen. Het gebruik van een reanimatieplank verbeterde de borstcompressiekwaliteit niet significant. Methodologisch sterk gerandomiseerde en gecontroleerde studies moeten uitgevoerd worden om deze bevindingen te bevestigen.
11 The master thesis is written in article format. The extended report of the systematic literature study is not part of the written article. The literature study was previously assessed in a similar course.
5
Introduction
“Cardiac arrest is the abrupt loss of heart function in a person who may or may not have been diagnosed with heart disease” (American Heart Association, 2017, p. 1). In the United States, there are yearly over 209.000 in-hospital cardiac arrests (IHCAs) in adult patients (Go et al., 2013). The presenting rhythm is most often (81%) non-shockable (asystole or pulseless electrical activity) (Andersen, Holmberg, Berg, Donnino, & Granfeldt, 2019). An incidence of 1.51 IHCAs per 1000 hospital admissions is described (Radeschi et al., 2017). In the United Kingdom Nolan et al. (2014) reported an incidence of 1.6 IHCAs per 1000 hospital admissions. In their article 14.784.144 hospital admissions were reported within two years, leading to 23.554 IHCAs. Of these, 16.9% were shockable rhythms (ventricular fibrillation or pulseless ventricular tachycardia) whereas non-shockable rhythms counted for 72.3%, with a survival rate after discharge of 49.0% and 10.5% respectively (Nolan et al., 2014).
Reported survival to hospital discharge following IHCA ranges from 0% to 42%, more commonly between 15% to 20% (Morrison et al., 2013; Sandroni, Nolan, Cavallaro, & Antonelli, 2007). High-quality cardiopulmonary resuscitation (CPR), specifically chest compressions, is essential to increase the likelihood of survival and enhance neurological outcome (Considine et al., 2020; Kleinman et al., 2015; Perkins et al., 2015). International guidelines of the European Resuscitation Council (ERC) for adult basic life support (BLS) were developed in collaboration with 22 international experts and recommend performing CPR on a firm surface when possible (Perkins et al., 2015).
However, IHCA usually happens in patients lying in hospital beds (i.e. not a firm surface). Transferring a patient to the floor cannot always be done safely and promptly (Handley, 2012). The International Liaison Committee on Resuscitation
12 (ILCOR) recommends not to move a patient from the hospital bed to the floor during IHCA (ILCOR, 2020). According to the ERC, chest compression quality during in-hospital CPR is often suboptimal on a soft surface (Monsieurs et al., 2015). Performing CPR on a mattress in bed results in mattress and bedframe deflection and negatively influences chest compression depth on the sternum during manikin CPR (Lin et al., 2017; Nishisaki et al., 2012; Noordergraaf et al., 2009; Oh, Kim, Kim, & Lee, 2016; Ruiz de Gauna, González-Otero, Ruiz, Gutiérrez, & Russell, 2016; Sainio et al., 2014). A reduction in chest compression depth of 31.1% by mattress compression has been observed (Lin et al., 2017). Other factors that might influence compression quality are e.g. bed height (Perkins, Benny, Giles, Gao, & Tweed, 2003; Perkins et al., 2006), sex (Amacher et al., 2017; Jaafar, Abdulwahab, & Al-Hashemi, 2015; Kaminska et al., 2018) and body mass index (BMI) (Jaafar, Abdulwahab, & Al-Hashemi, 2015; Klickovic et al., 2012; Krikscionaitiene et al., 2010).
Focusing on mattress compression, a backboard can be placed between the patient and the mattress to reduce its unfavourable effect on chest compression quality. Overall, a lack of evidence exists on the use and effectiveness of a backboard during in-hospital CPR. A recent manikin study observed an increase in compression quality (Sanri & Karacabey, 2019), while other manikin studies reported no improvement in compression quality when using a backboard during CPR on a mattress (Fischer, Mayrand, & Ten Eyck, 2016; Perkins et al., 2006; Putzer et al., 2016; Schober et al., 2014). Some authors described a decrease in mattress compressibility but emphasised that it is not eliminated (Lin et al., 2017; Noordergraaf et al., 2009; Oh, Kim, Kim, & Lee, 2016). Furthermore, the placement of a backboard during in-hospital CPR interrupts the resuscitation cycle and might lead to dislocation of catheters (Perkins et al., 2015).
The lack of international guidelines concerning the effectiveness of a backboard could be due to methodological differences between studies. The current practice is primarily focused on chest compression depth, while chest compression quality is determined by compression depth, compression rate and chest recoil (Perkins
13 et al., 2015). However, evidence is necessary to develop and implement good practices of a backboard during in-hospital CPR.
The aim of this study was to evaluate the effect of a backboard on chest compression depth, compression rate and chest recoil during in-hospital CPR on an adult-sized manikin. Sex, BMI, age and department were considered as potential confounders.
14
6
Methods
This study hypothesised that backboard use could enhance compression depth, rate and chest recoil. Compression force on the manikin torso is spread over a larger surface on the mattress. Therefore, an increase in mattress stiffness, a reduction in mattress compression and thus an increase in actual chest compression depth on the sternum was assumed (Boe & Babbs, 1999).
6.1 Study design
A prospective, non-crossover, superiority trial was conducted between mid-October 2019 and February 2020. A superiority design was chosen since backboard CPR needed to be superior to CPR without a backboard in order to risk interrupting compressions. This randomised controlled trial (RCT) was reported in accordance with the 2010 CONSORT statement and extensions for simulation-based research (Cheng et al., 2016).
6.2 Setting and sample
In a Flemish general hospital with 810 beds (Belgium) a consecutive sample was selected, based on following inclusion criteria: (i) licenced nurse and (ii) working in adult critical or non-critical care. Minimal work experience or recent CPR qualification was not required. Head nurses of the hospital were informed about the study during the monthly meeting and informed their staff afterwards. Participants were invited to participate by poster (Appendix 1), mail, telephone and face-to-face contact on the ward.
6.3 Intervention
Participants were provided with CPR training (phase one: six weeks) prior to the intervention (phase two: nine weeks).
15
6.3.1 Phase one
CPR training was provided with a CPR self-learning station (CPRTEST®, Pinga Group, Belgium) using a repetitive formative test strategy. This validated training strategy provided standardised and objective CPR training and reduced the impact of instructor bias (Mpotos, De Wever, Valcke, & Monsieurs, 2012; Mpotos et al., 2013; Mpotos et al., 2015). Since participants were familiar with instructed manikin CPR but not with automated self-learning and assessment of CPR skills, a non-obstructive instructor was always present. The CPR self-learning station consisted of a laptop connected to a new adult-sized manikin torso (15.75kg, Resusci Anne®, Laerdal, Norway). The manikin was equipped with an internal CPRTEST® sensor (Pinga Group, Belgium) to record compression and ventilation parameters.
First, participants were asked to log into the CPRTEST® software (Pinga Group, Belgium). A brief written summary was presented of the 2015 ERC guidelines concerning chest compression depth, rate, recoil and ventilation volume as well as the pass criteria. In order to pass the training, participants had to achieve a predefined combined CPR score of ≥70%: ≥70% chest compressions with depth 50-60mm and ≥70% chest compressions with complete release (≤5mm) and a mean compression rate of 100-120bpm and ≥70% ventilations with a visible chest rise (volume 200-800ml). Past research recommended clinical competence to be assured by passing a predefined competence level (Wass, Van der Vleuten, Shatzer, & Jones, 2001). When reaching the combined CPR score, participants obtained a CPR certificate. In accordance with previous research testing this CPR training strategy, the threshold of ≥70% was arbitrarily chosen (Mpotos et al., 2013; Mpotos et al., 2015).
Next, a short CPR scenario was presented to the participants followed by an analogue clock and digital countdown timer of ten seconds to prepare for resuscitation. An auditive signal indicated the start of the test. Participants were asked to perform two minutes of BLS (five cycles with a compression-to-ventilation (C:V) ratio of 30:2) according to the 2015 ERC guidelines. Training in
16 phase one was executed on the floor. Compressions always had to be performed by the participants. For the ventilations one of the researchers performed a head tilt and chin lift and held a bag-valve-mask in place so the participant could ventilate the manikin. After two minutes an auditive signal indicated the end of the test.
During the formative CPR test (simulation) there was no audio-visual feedback. Providing feedback during CPR would likely make shallow compressions uncommon and therefore not representative for CPR in the real clinical practice. Participants only saw an analogue clock and digital countdown timer of two minutes. After the test feedback was automatically provided to every participant and when the pass criteria were not achieved feedforward was given to improve the participant’s performance (Appendix 2). There was no limitation to the number of training efforts a person could perform to achieve a combined CPR score of ≥70%. Every new training effort started with feedback of the last CPR test and feedforward to improve during this new test. To minimise bias due to an unequal baseline CPR skill level, only nurses who achieved the predefined combined CPR score ≥70% in phase one were enrolled in phase two.
6.3.2 Randomisation
Participants who obtained a combined CPR score ≥70% in phase one were alphabetically listed by surname and then randomised (block size = 10, allocation ratio 1:1) into two groups by an online randomisation tool (Sealed Envelope Ltd., 2020): a backboard group and a control group. The first generated randomisation list was automatically the final one.
6.3.3 Phase two
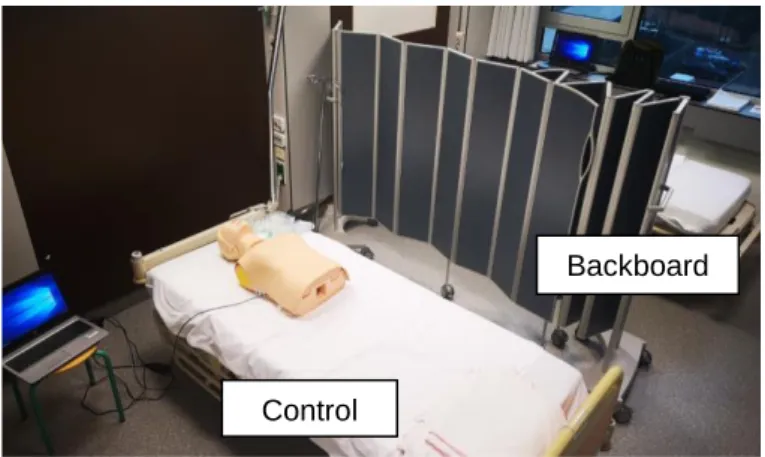
Phase two was conducted in a room with two hospital beds (Evolution™ LI-156E0, Hill-Rom®, The Netherlands) separated by a screen. On each bedframe a new memory foam mattress (200 x 90 x 14 cm, VISCOSAM85®, Sampli, Belgium) was placed with a density of 80-85kg/m³ (top layer, 4 cm) and 50-55kg/m³ (bottom layer, 10 cm). A manikin torso (15.75kg, Resusci Anne®, Laerdal, Norway), as
17 used in phase one, was placed on each mattress (Figure 1). Both manikins were identical and equipped with a validated and patented CPRTEST® sensor (EP 3370220, Pinga Group, Belgium). The internal sensor automatically measured chest compression depth (adjusted for mattress deflection), chest recoil, compression rate and ventilation volume. In each manikin calibration of the sensor occurred at the start of every new CPR test to provide reliable test results. The CPRTEST® software (Pinga Group, Belgium) registered all data from the sensor in a database.
Figure 1: Phase two general setup
Both beds were placed in the lowest position. In the backboard group, a backboard (59 x 44 x 5 cm, 2kg, CPR board, Bound Tree Medical, Dublin, OH, USA) was placed in a longitudinal (head to toe) orientation between the manikin and the mattress. To ensure blindness of the participants, the mattress and the backboard (if present) were covered with a non-translucent white sheet (Figure 2) and a non-obstructive researcher was present throughout phase two. None of the participants were informed about the use and evaluation of a backboard. Participant’s spontaneous remarks about the presence or absence of a backboard were counted.
Backboard group
Control group
18
Figure 2: Backboard group setup
To test the study hypothesis, a new CPR test (two minutes, C:V ratio of 30:2) had to be performed in phase two. Participants were instructed to perform only one CPR test (regardless of the achieved combined CPR score) and position themselves as they would while performing real-life CPR in bed. CPR was performed in the same manner as in phase one. After the CPR test, participants were given feedback and completed the data collection process. A successful CPR test in phase two was achieved when a combined compression score of ≥70% was reached: ≥70% chest compressions with depth 50-60mm and ≥70% chest compressions with complete release (≤5mm) and a mean compression rate of 100-120bpm. This score was manually calculated after data collection using the same approach as the combined CPR score by the software in phase one: the lowest percentage on all compression parameters (depth, rate and chest recoil) determined the percentage of the combined compression score.
Backboard Memory foam mattress CPR manikin with internal CPRTEST® sensor
19 6.4 Outcome measures and covariates
The primary outcomes were defined as the difference in proportion of participants achieving (i) a combined compression score ≥70%, (ii) ≥70% chest compressions with depth 50-60mm, (iii) ≥70% chest compressions with complete release (≤5mm) and (iv) a mean compression rate of 100-120bpm between both study groups. Secondary outcomes were defined as the difference in median (i) chest compression depth, (ii) compression rate and (iii) number of compressions with complete release between both study groups.
The covariates considered were sex, age (21-30 years, 31-40 years, 41-50 years, ≥51 years), department (critical care, non-critical care) and BMI (<25 kg/m², 25-30 kg/m², >25-30kg/m²). Together with the time since last CPR training the previous four demographic variables were registered in every participant after the first login into the software.
6.5 Sample size calculation
A 10% difference in the proportion of participants reaching the ≥70% combined compression score between both study groups was predefined as clinically relevant. SAS® Power and Sample Size (Version 9.4, SAS Institute Inc., Cary, NC, USA) was used to calculate the required sample size. A sample size of 250 participants per group was required to detect a 10% difference between the backboard group (85% achieving threshold ≥70%) and control group (75% achieving threshold ≥70%), (β=0.80 and α=0.05). High success rates were expected since CPR skills deteriorate within three to twelve months after BLS training (Greif et al., 2015). The maximum time interval between phase one and two was initially expected to be two months. The total sample size was doubled (n=1000) considering a dropout of 50% between phase one and two was anticipated. Since it seemed unlikely that the desired sample size would be achieved during the study period, a post hoc power calculation was anticipated.
20 6.6 Statistical methods
Compression quality is the major determinant for survival (Considine et al., 2020; Kleinman et al., 2015; Perkins et al., 2015) and the primary outcome in this study. Therefore, researcher assisted ventilations were not included in data-analysis in phase two. A two-sided p-value set at α < 0.05 was considered statistically significant.
Chi-square and Fisher's exact tests were used in categorical variables (reported as rates and counts) to assess the effect of a backboard on the four primary outcomes. Mann-Whitney U tests were used in non-normally distributed continuous variables (reported as medians and interquartile ranges (IQR)) to assess the effect of a backboard on the three secondary outcomes.
Multiple logistic regression analyses were executed to assess independent relationships with the four primary outcomes. Independent variables in these analyses included BMI, age, sex and department. The ‘Enter’ method was used and covariates with p>0.15 were stepwise removed from the model. The Hosmer-Lemeshow test was performed to estimate the goodness-of-fit of the regression models (Hosmer, Lemeshow, & Sturdivant, 2013). Since there was no difference in the primary outcomes between participants in the first three age categories, the covariate was recoded into two categories (21-50 years and ≥51 years) and analysed using IBM® SPSS® Statistics (Version 25.0, IBM Corporation, New York, NY, USA).
6.7 Ethical considerations
The study protocol was approved by the Ethics Committee of Ghent University Hospital, Ghent, Belgium (trial registration B670201941133). Digital informed consent was obtained from every participant. Written informed consent was additionally obtained from every participant in phase two (Appendix 3). All study procedures were performed according to the Good Clinical Practice Guidelines (ICH/GCP) and the ethical guidelines of the Helsinki Declaration (2013 version).
21
7
Results
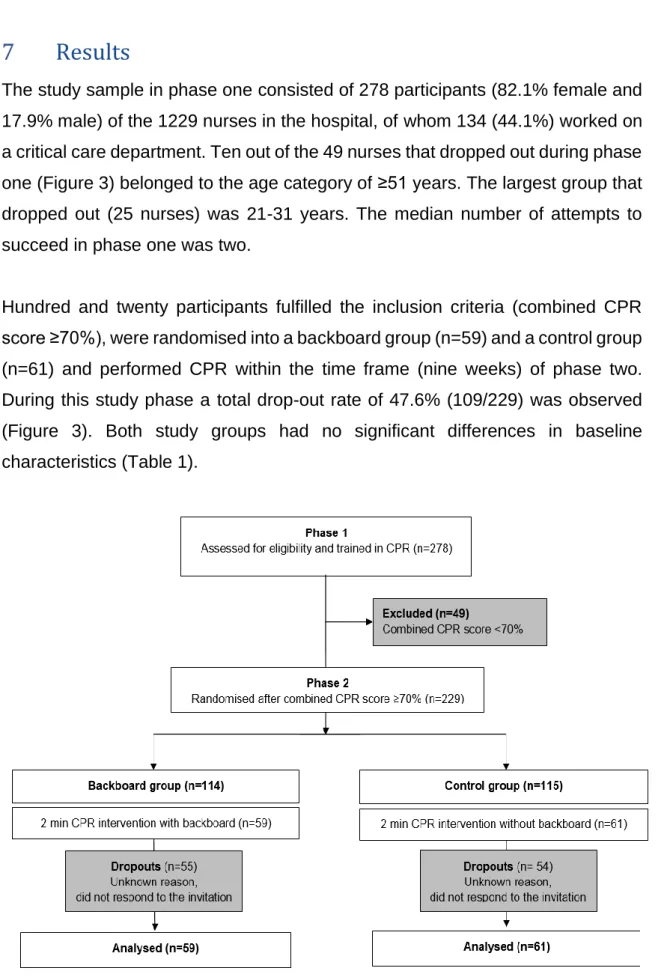
The study sample in phase one consisted of 278 participants (82.1% female and 17.9% male) of the 1229 nurses in the hospital, of whom 134 (44.1%) worked on a critical care department. Ten out of the 49 nurses that dropped out during phase one (Figure 3) belonged to the age category of ≥51 years. The largest group that dropped out (25 nurses) was 21-31 years. The median number of attempts to succeed in phase one was two.
Hundred and twenty participants fulfilled the inclusion criteria (combined CPR score ≥70%), were randomised into a backboard group (n=59) and a control group (n=61) and performed CPR within the time frame (nine weeks) of phase two. During this study phase a total drop-out rate of 47.6% (109/229) was observed (Figure 3). Both study groups had no significant differences in baseline characteristics (Table 1).
22
Table 1: Demographics participants phase two Variable Backboard Groupa
(n=59)
Control group b
(n=61)
p-value
Median (IQR) / n (%) Median (IQR) / n (%)
Age (years) 37.00 (28.00-45.00) 35.00 (27.00-48.00) 0.737 d Critical vs. non-critical care department 26 (44.1) vs. 33 (55.9) 27 (44.3) vs. 34 (55.7) 0.983 c Sex (male) 15 (25.4) 12 (19.7) 0.451 c BMI 23,03 (20.93-25.88) 23.83 (21.31-28.07) 0.265 d Legend:
a Intervention: With backboard
bControl: Without backboard
c Chi-square test.
23 7.1 Effect of a backboard
No significant difference was found between both groups in achieving a combined compression score of ≥70% in phase two (Table 2). In total, only 53 participants achieved a combined compression score of ≥70%. Out of the 24 nurses with an age of ≥51 years in phase two, only four passed this predefined threshold. Between both study groups, no difference was observed regarding compression depth, chest recoil and compression rate (Table 2). Graphic representations of these results can be found in Figure 4 and 5.
Table 2: Proportions of successful participants Variable Backboard Groupa
n/N (%) [95% CI] Control group b n/N (%) [95% CI] p-value c ≥70% compressions with depth 50-60 mm 37/59 (62.7) [50.0-75.0] 31/61 (50.8) [38.0-64.0] 0.189 ≥70% compressions with complete release (≤5 mm) 57/59 (96.6) [92.0-100.0] 57/61 (93.4) [87.0-100.0] 0.426
Mean compression rate 100–120 min−1 44/59 (74.6) [63.0-86.0] 49/61 (80.3) [70.0-91.0] 0.451 ≥70% combined compression score d 28/59 (47.5) [34.0-61.0] 25/61 (41.0) [28.0-54.0] 0.475 Legend:
a Intervention: With backboard
bControl: Without backboard
c Chi-square test.
d 70% combined compression score: ≥70% of all compressions 50-60mm and ≥70% of all compressions
24
Figure 4: Graphical representation of successful participants – Combined compression score and chest compression depth
25
Figure 5: Graphical representation of successful participants – Chest compression rate and chest recoil
With a sample size of 59 (backboard group) and 61 (control group), a significance level of 0.05 and a proportion of participants reaching the threshold of ≥70% combined compression score in phase two of 47.5% (backboard group) and 41.0% (control group), the post hoc power analysis resulted in a power of 0.083.
26 In comparing the median chest compression depth, rate and chest recoil between both groups no statistically significant difference was found (Table 3). Furthermore, 23.7% of the backboard group noted the presence of a backboard. However, 21.3% of the control group stated spontaneously that a backboard needed to be placed in order to perform high quality CPR on a memory foam mattress.
Table 3: Median of chest compression parameters Variable Backboard Group a
(n=59)
Control group b
(n=61)
p-value c
Median (IQR) Median (IQR)
Compression depth (mm) 52.82 (49.57-56.16) 52.86 (48.95-57.08) 0.815 Median number of compressions with complete release 163.49 (150.50-180.00) 162.93 (159.50-180.00) 0.778 Compression rate (bpm) 107.86 (102.00-117.00) 108.28 (102.50-116.00) 0.866 Legend:
a Intervention: With backboard
bControl: Without backboard
27 7.2 Influence of age, sex, BMI and department
A multiple binary logistic regression analysis was performed to assess independent relationships with combined compression score (Table 4). The Hosmer and Lemeshow statistic indicated no significant difference between the observed and expected values (p=0.925). Only age was a significant predictor. Participants 51 years or older were significantly less likely to achieve the combined compression score compared to younger participants.
The logistic regression model could not identify any independent predictors for the individual score component ‘chest compression depth’. As for chest recoil, only the group participants 51 years or older performed significantly lower compared with their younger colleagues. For what concerns ‘chest compression rate’, participants of non-critical care departments were a significant predictor for poor chest compression rate. No other variables reached statistical significance.
Additionally, table 4 shows that a backboard was not a significant predictor for any of the four dependent variables.
28
Table 4: Final predictors for successful chest compression quality Dependent Variable Predictor p-value Odds
Ratio 95% C.I. Lower Upper Combined compression score Backboard, yes 0.522 1.288 0.593 2.800 Department, critical care 0.076 2.038 0.929 4.473 Age, ≥51 0.002 0.133 0.037 0.479 Sex, male 0.113 2.352 0.817 6.768
Hosmer and Lemeshow test: p = 0.925
Chest compression depth Backboard, yes 0.215 1.589 0.764 3.308 Sex, male 0.268 1.666 0.675 4.117
Hosmer and Lemeshow test: p = 0.481
Chest recoil Backboard, yes 0.382 2.290 0.358 14.668 Age, ≥51 0.004 0.038 0.004 0.352
Hosmer and Lemeshow test: p = 0.770
Chest compression rate Backboard, yes 0.470 0.719 0.294 1.758 Department,
critical care
0.036 2.818 1.071 7.416 Age, ≥51 0.060 0.381 0.140 1.039
Hosmer and Lemeshow test: p = 0.102 Legend:
Predictors with p>0.15 were stepwise removed from the model (except “backboard”) as long as at least two predictors per dependent variable remained in the final model.
Analysis is based on logistic regression. P-values <0.05 are considered statistically significant. P-values with range of 0.05-0.10 are considered a trend to significance.
29
8
Discussion
8.1 Effect of a backboard
This manikin study evaluated the effect of a backboard on chest compression quality. No significant differences in chest compression depth, chest recoil and compression rate were found when CPR-certified nurses performed chest compressions with or without a backboard on a memory foam mattress. The logistic regression model confirmed this result by showing that a backboard was not a significant predictor for any of the four dependent variables.
A lack of evidence exists around the effectiveness of a backboard during in-hospital adult CPR. Moreover, existing evidence only consists of manikin studies. However, a number of methodological differences between these studies are observed such as mattress type and thickness, sample size and composition, CPR duration, weight of the manikin, size and orientation of the backboard, position of the participant during CPR, outcome measure, target compression depth/recoil/rate and whether or not participants were blinded or given feedback during CPR. Therefore, comparing study results about the effectiveness of a backboard is not obvious. Extrapolating manikin results to humans also remains complicated and limited. Moreover, previous manikin studies were generally focused on mean chest compression depth, while chest compression quality is determined by chest compression depth, compression rate and chest recoil (Perkins et al., 2015). In addition, means are not robust and are sensitive for every single outlier, while medians tolerate up to 50% of outliers (Fabozzi, Focardi, Rachev, & Arshanapalli, 2014; Ripley, 2005; Rousseeuw & Hubert, 2011).
The study of Sanri and Karacabey (2019) was methodologically closest to our trial by investigating the effect of a backboard on all three components (compression depth, chest recoil and compression rate) of total chest compression quality. Their manikin study evaluated the effect of a backboard on a stretcher with an 8-cm foam mattress in 101 medical students. In the backboard group a significant improvement for every individual compression parameter was observed. The proportion of compressions with all three sub-parameters being successful
30 increased from 38.0% to 66.7% (Sanri & Karacabey, 2019). When compared to this current study, those better results might be attributed to differences in mattress thickness or the absence of a pretest. Our RCT used a 14-cm thick foam mattress, which could have induced a higher compressibility, faster fatiguing and therefore a higher risk of insufficient chest compressions. With regard to the pretest, all participants received CPR training during their emergency medicine clerkship in the study of Sanri and Karacabey (2019). However, no measurement is reported of their actual competence level after training. Hence, the significant improvement in chest compression quality due to a backboard might also be explained by an unequal baseline CPR skill level in the intervention and control group.
The effectiveness of a backboard on chest compression depth is influenced by mattress stiffness (ILCOR, 2020) and mainly described in soft mattresses, not in relatively hard1 hospital mattresses (Andersen, Isbye, & Rasmussen, 2007; Cloete, Dellimore, Scheffer, Smuts, & Wallis, 2011; Fischer, Mayrand, & Ten Eyck, 2016; Nishisaki et al., 2012; Oh, et al., 2013b; Perkins, Kocierz, Smith, McCulloch, & Davies, 2009; Sanri & Karacabey, 2019). A standard hospital mattress typically has a stiffness of 100-200 N/cm (Cloete, Dellimore, Scheffer, Smuts, & Wallis, 2011; Dellimore, Cloete, & Scheffer, 2011). One manikin study concluded that the compression quality significantly increased when using a backboard on a surface with <250N/cm back support stiffness, while the advantage of backboard use decreased in higher stiffness surfaces (Cloete, Dellimore, & Scheffer, 2011b). This can be explained by a higher amount of mattress compressibility in soft mattresses and therefore a greater opportunity for chest compression optimisation when using a backboard. However, three manikin studies with foam and/or pressure relieving mattresses did not support the use of a backboard during CPR (Perkins et al., 2006; Putzer et al., 2016; Schober et al., 2014) and are similar to our findings. In two manikin studies conducted on
1 Relatively hard hospital mattresses were defined as emergency stretcher mattresses,
operating room mattresses and more dense standard hospital mattresses (as reported according to the study). Density of the different mattresses was not reported in every study. Therefore, this classification was created.
31 relatively hard mattresses2 (6-cm Softnurse® pressure-distributing operating room mattress and 7.5-cm Sure-Chek® Stretcher Pad emergency department mattress) the use of a backboard during CPR was supported (Cheng, Belanger, Wan, Davidson, & Lin, 2017; Sato et al., 2011). However, both study samples consisted of respectively 70% and 100% males which could have introduced bias on the study results.
Apart from mattress stiffness, the effectiveness of a backboard on chest compression quality is also influenced by the backboard’s orientation and size (ILCOR, 2020). In this study only one backboard size and orientation (longitudinal) were assessed. This backboard size corresponds to the small backboard sizes used in several manikin studies (Cloete, Dellimore, & Scheffer, 2011a; Cloete, Dellimore, Scheffer, Smuts, & Wallis, 2011; Nishisaki et al., 2012). A longitudinal backboard orientation increases compression stiffness compared to a latitudinal orientation (Cloete, Dellimore, & Scheffer, 2011a), however when using a smaller backboard orientation seems less significant (Cloete, Dellimore, Scheffer, Smuts, & Wallis, 2011). Despite Nishisaki et al. (2012) stating that backboard orientation and size does not significantly influence mattress displacement, a large backboard (86 x 50 cm) was regardless of orientation significantly associated with deeper chest compressions than a small backboard in the study of Cloete, Dellimore, Scheffer, Smuts and Wallis (2011). This might be an explanation for the observed non-superiority of a backboard in the present study.
The continuing existence of mattress compression despite using a backboard might be another possible explanation for our findings. Three manikin studies observed reduced mattress compression using a backboard, but emphasise that it is not eliminated (Lin et al., 2017; Noordergraaf et al., 2009; Oh, Kim, Kim, & Lee, 2016). Perkins, Kocierz, Smith, McCulloch and Davies (2009) hypothesised that this is the result of a backboard not being fixed to a stable external structure. Another hypothesis could be shifting of the backboard during chest compressions. This could subsequently result in a seesaw effect where the area of the backboard
32 in contact with the underlying mattress is decreased during the delivery of a chest compression (Perkins, Kocierz, Smith, McCulloch, & Davies, 2009). Therefore, the provided back support stiffness could be lower and performing adequate chest compressions could be more difficult.
Furthermore, the expected sample size in phase two was not reached within the limited study time frame. Reasons for dropout in phase one (n=49) could have been the inability to perform enough adequate compressions due to limited muscle strength or fatigue, lack of motivation since the threshold for passing CPR training in the hospital is set lower or lack of time to perform multiple training sessions due to workload on the ward. Despite a short time investment (two minutes of CPR) and frequent reminders, a dropout rate of 47.6% was observed in phase two. This could be explained by the fact that phase two was not part of the hospital’s CPR training programme and CPR certification could not be renewed. Heavy workload on the ward might be another explanation.
Considering the results of this current trial it is worth looking at other strategies than a backboard to improve chest compression quality during CPR on a mattress in bed. Some alternatives may be a CPR foam mattress that can be compressed during CPR with a vacuum pump (Delvaux et al., 2009), a mattress compression cover with vacuum pump (Oh et al., 2013a), dual accelerometer feedback during CPR (ILCOR, 2020) or training to/providing deeper chest compressions than recommended during CPR in bed (Handley, 2012; ILCOR, 2020; Oh et al., 2016). If present, the ILCOR recommends activating CPR mode of a bed to increase mattress stiffness (ILCOR, 2020).
To assess the effect of a backboard on chest compression quality, both medians and proportions were reported. Only reporting medians would provide less information than reporting proportions of participants who achieved the ≥70% threshold (Mpotos, 2013). Moreover, according to Mpotos et al. (2015) reporting a combined competence score acknowledges more comprehensive reporting of the total CPR quality than individual reporting of each CPR skill (Mpotos et al.,
33 2015). The results of the present study confirm this previous statement: based on the proportion of participants obtaining the threshold for compression depth, chest recoil and compression rate individually, both study groups consistently scored above 50%. However, the proportion of participants obtaining a combined compression score ≥70% was less than 50% in both study groups, despite recent CPR training. It is known that CPR skills already deteriorate within three to twelve months after BLS training (Greif et al., 2015). In this study the interval between phase one and two could reach a maximum of 3.5 months. However, there are other potential explanations for the observed shallow CPR performance.
Participants were trained to a predefined combined CPR score on the floor during phase one and performed the CPR test in phase two on a mattress in bed. Successful chest compressions during manikin CPR training on the floor (without feedback) did not guarantee successful chest compressions during manikin CPR in bed (without feedback). A different CPR position (kneeling on a stable floor vs. standing next to or kneeling in a less stable bed) and the unfavourable influence of mattress deflection on compression depth during CPR in bed are two major factors that could indicate the impact of fatigue and explain low success rates in phase two (Hasegawa, Okane, Ichikawa, Inukai, & Saito, 2020; Lin et al., 2017; Nishisaki et al., 2009; Noordergraaf et al., 2009; Oh, Kim, Kim, & Lee, 2016; Ruiz de Gauna, González-Otero, Ruiz, Gutiérrez, & Russell, 2016; Sainio et al. 2014). Focusing on compression depth, four manikin studies are in line with this study result and observed a higher mean/median compression depth on the floor than on a stretcher or hospital bed with foam/pressure relieving mattress (Hasegawa, Okane, Ichikawa, Inukai, & Saito, 2020; Jang et al., 2009; Sebbane et al., 2012; Tweed, Tweed, & Perkins, 2001). However, there is also evidence stating that there is no difference in compression depth between CPR on the floor and CPR in bed (Ahn et al., 2019; Jäntti, Silfvast, Turpeinen, Kiviniemi, & Uusaro, 2009; Mygind-Klausen et al., 2018; Oh, Kim, Kim, Lee, & Lee, 2014; Perkins, Benny, Giles, Gao, & Tweed, 2003; Schober et al., 2014).
34 Another explanation for the low success rates in phase two might be reduced mattress pre-compression. Pre-compression could induce a higher density of the mattress and lead to reaching compressions of adequate depth more easily. In the current study new mattresses were used to avoid mattress pre-compression due to prolonged use. In addition, the lower torso weight of the manikin does not match the actual weight of an adult patient’s torso and could induce less mattress pre-compression. This leaves more potential for mattress deflection during CPR. This assumption is in line with the manikin study of Nishisaki et al. (2012), stating that a lighter torso weight (25kg) was related to more mattress deflection in a 14-cm Hill-Rom® therapy mattress on an ICU bed (Nishisaki et al., 2012). It is possible that, despite their clinical expertise, nurses were not able to adjust to more mattress deflection in the present study in comparison to real life CPR of an adult on a mattress. However, Noordergraaf et al. (2009) stated that the effects of adding weight were rather small (Noordergraaf et.al, 2009).
35 8.2 Influence of age, sex, BMI and department
This current study found that only age predicted a higher chance of failing to achieve the ≥70% combined compression score. For the individual scores (chest compression depth, chest recoil and compression rate) only age ≥51 years was a significant predictor for not achieving ≥70% chest recoil. However, the age group of ≥51 years did show a trend to significance to predict a mean compression rate of 100-120bpm. This is in line with the findings of Peberdy, Silver and Ornato (2009) where individuals of ≥51 years achieved a lower mean chest compression depth and a higher percentage of suboptimal chest compressions than younger individuals (Peberdy, Silver, & Ornato, 2009). This could be due to a loss of muscle mass and strength with ageing. However, the participants performed CPR on a firm table and not on a mattress.
With regard to sex (males) and BMI (<25) this current study could not demonstrate an impact on achieving a combined compression score of ≥70%. Yet, other studies suggested that sex (Amacher et al., 2017; Jaafar, Abdulwahab, & Al-Hashemi 2015; Peberdy, Silver, & Ornato, 2009) and BMI (Gianotto-Oliveira et al., 2010; Jaafar, Abdulwahab, & Al-Hashemi 2015; Sayee & McCluskey, 2012) are significant predictors for adequate chest compression quality. Two studies stated that males performed better than females on CPR quality (Amacher et al., 2017; Peberdy, Silver, & Ornato, 2009), but the ratio of male/female participants was not evenly distributed in their study which could have overestimated the outcomes. Jaafar, Abdulwahab and Al-Hashemi (2015) reported that participants with a mean BMI of <26 performed better than those with a mean BMI of >26 (Jaafar, Abdulwahab, & Al-Hashemi, 2015), whereas other studies stated that healthcare providers with a higher BMI were associated with better CPR quality (Gianotto-Oliveira et al., 2010; Sayee & McCluskey, 2012). According to Kaminska et al. (2018) there is an indication that basal metabolic rate, fat-free mass, trunk muscle mass and left and right muscle mass better correlates to compression depth and rate than BMI (Kaminska et al., 2018).
36 The critical care departments showed a trend to significance to predict a combined compression score of ≥70%. Belonging to a non-critical care department was a significant predictor for not achieving a compression rate of 100-120bpm. Guidelines from the ERC state that CPR retraining should be performed every twelve to twenty-four months (Greif et al., 2015). Critical care departments are usually trained in BLS every year, whereas the non-critical care departments are trained every two years. Taking this into account, there was an assumption that the critical care department performed BLS more correctly. However, there was little to no evidence that supported this statement.
37 8.3 Recommendations for clinical practice and further research
Since CPR using a backboard is not significantly superior to CPR without a backboard, this manikin study suggests against the interruption of chest compressions to place a backboard. However, the generalizability of our results is limited and therefore CPR teams should carefully assess whether placing a backboard is justified for the type of mattresses used in their hospital (Schober et al., 2014). Further well-designed, multicenter RCT’s on all three compression parameters (compression depth, chest recoil and compression rate) are necessary using other types of bed frames, mattresses, backboards or backboard positions.
Clinical outcome studies are required since there is no evidence identified to date on the effect of a backboard on critical outcomes as return of spontaneous circulation (ROSC), survival and favourable neurological outcome (ILCOR, 2020).
Finally, this study confirms the need for more frequent CPR retraining as recommended by the ERC and suggests more frequent CPR training and education programmes for nurses ≥51 years old. Yearly retraining may be insufficient given that CPR skills already decay within months after training (Greif et al., 2015). However, since the number of analysed nurses ≥51 years old was small (n=24) and the trial was monocentric, the generalizability of these results is limited.
38 8.4 Study limitations
This study has several limitations. First, the sampling method is not random, implying a greater chance of sampling bias. Furthermore, the calculated sample size was not reached. Therefore, it became improbable to demonstrate a significant difference between the groups. However, a post hoc power calculation revealed a β=0.08 indicating unlikeliness of finding significant differences even when the anticipated sample size would have been achieved. For the observed difference to be statistically significant a sample size of 1832 participants would have been required. Second, the level of fatigue was not assessed in this study. Quantifying the level of fatigue on the floor and in bed with a self-reporting scale could have provided more insight. Two minutes of CPR may be insufficient to detect fatigue. In defence, every two minutes the cardiac rhythm is analysed and according to the 2015 ERC guidelines the provider of compressions is preferably switched to prevent fatigue (Monsieurs et al., 2015). Third, blinding a backboard is questionable as one can feel its presence during CPR. However, since using a backboard during CPR in bed was standard in the hospital, participants in the backboard group would likely not question the presence of a backboard and therefore the true objective of the study.
Fourth, considering this trial was conducted with manikins, extrapolation of the results to patients in the clinical field remains limited. Fifth, despite the bed in phase two being in the lowest position for each participant, there was no standardisation in the participant’s position relative to the bed (standing next to vs. kneeling in bed). This variable was not assessed but a notable difference between both study groups could have influenced the achieved results. Sixth, only one type of manikin, bed frame, mattress, backboard, backboard size and backboard orientation in one hospital was tested. This limits the generalizability of the study. Seventh, since the study was single-blinded time loss in backboard placement could not be evaluated. A mean time loss of 10.6 ± 4 seconds was previously observed in a CPR team of three persons (Perkins et al., 2006). Additionally, mattress compressibility was not measured given that the clinical
39 relevance for CPR lies in the effective compression depth performed on the sternum and not directly in the amount of mattress compression.
40
9
Conclusion
In accordance to the ERC guidelines (2015), no significant differences in chest compression depth, rate and chest recoil were found when CPR-certified nurses performed chest compressions with or without a backboard on a memory foam mattress during manikin CPR. This should be interpreted in view of a test phase that lasted for only two minutes, implying likely minimal effect of fatigue.
BMI, sex and department were not statistically significant predictors for achieving a combined compression score of ≥70%. Nurses ≥51 years old were less likely to achieve the threshold of ≥70% compared to younger nurses. Therefore, this group of nurses might benefit from more frequent CPR training and education programmes to improve CPR quality and performance and therefore increase chances for survival from sudden IHCA.
This manikin study could not identify any independent predictors for the individual compression component ‘chest compression depth’. Only CPR-certified nurses ≥51 years old performed significantly lower chest recoil during in-hospital manikin CPR compared to younger nurses. Concerning chest compression rate, CPR-certified nurses from non-critical care departments performed significantly poorer chest compression rate during in-hospital manikin CPR than nurses from critical care departments.
41
10
References
Ahn, H. J., Cho, Y., You, Y. H., Min, J. H., Jeong, W. J., Ryu, S., … Choi, Y. (2019). Effect of using a home-bed mattress on bystander chest compression during out-of-hospital cardiac arrest. Hong Kong Journal of Emergency Medicine. doi:10.1177/1024907919856485
Amacher, S. A., Schumacher, C., Legeret, C., Tschan, F., Semmer, N. K., Marsch, S., & Hunziker, S. (2017). Influence of Gender on the Performance of Cardiopulmonary Rescue Teams: A Randomized, Prospective Simulator
Study. Crit Care Med, 45(7), 1184-1191.
doi:10.1097/CCM.0000000000002375
American Heart Association (2017). About Cardiac Arrest. Retrieved from
https://www.heart.org/en/health-topics/cardiac-arrest/about-cardiac-arrest
Andersen, L.Ø, Isbye, D. L., & Rasmussen, L. S. (2007). Increasing compression depth during manikin CPR using a simple backboard. Acta anaesthesiologica Scandinavica, 51(6), 747-750. doi:10.1111/j.1399-6576.2007.01304.x
Andersen, L. W., Holmberg, M. J., Berg, K. M., Donnino, M. W., & Granfeldt, A. (2019). In-Hospital Cardiac Arrest: A Review. JAMA, 321(12), 1200-1210. doi:10.1001/jama.2019.1696
Boe, J. M., & Babbs, C. F. (1999). Mechanics of cardiopulmonary resuscitation performed with the patient on a soft bed vs a hard surface. Academic emergency medicine, 6(7), 754-757. doi:10.1111/j.1553-2712.1999.tb00449.x
Cheng, A., Belanger, C., Wan, B., Davidson, J., & Lin, Y. (2017). Effect of Emergency Department Mattress Compressibility on Chest Compression Depth Using a Standardized Cardiopulmonary Resuscitation Board, a Slider Transfer Board, and a Flat Spine Board: A Simulation-Based Study. Simulation in healthcare : journal of the Society for Simulation in Healthcare, 12(6), 364-369. doi:10.1097/SIH.0000000000000245
Cheng, A., Kessler, D., Mackinnon, R., Chang, T. P., Nadkarni, V. M., Hunt, E. A., …Auerbach, M. (2016). Reporting guidelines for health care simulation
42 research: extensions to the CONSORT and STROBE statements. Advances in simulation, 1(1), 25. doi:10.1186/s41077-016-0025-y
Cloete, G., Dellimore, K., & Scheffer, C. (2011a). The impact of various backboard configurations on compression stiffness in a manikin study of CPR. Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2484-2487.
Cloete, G., Dellimore, K. H., & Scheffer, C. (2011b). Comparison of experimental chest compression data to a theoretical model for the mechanics of constant peak displacement cardiopulmonary resuscitation. Academic Emergency Medicine, 18(11), 1167-1176. doi:10.1111/j.1553-2712.2011.01213.x
Cloete, G., Dellimore, K. H., Scheffer, C., Smuts, M. S., & Wallis, L. A. (2011). The impact of backboard size and orientation on sternum-to-spine compression depth and compression stiffness in a manikin study of CPR using two mattress types. Resuscitation, 82(8), 1064-1070. doi:10.1016/j.resuscitation.2011.04.003
Considine, J., Gazmuri, R. J., Perkins, G. D., Kudenchuk, P. J., Olasveengen, T. M., Vaillancourt, C., ... Morley, P. (2020). Chest compression components (rate, depth, chest wall recoil and leaning): A scoping review. Resuscitation, 146, 188-202. doi:10.1016/j.resuscitation.2019.08.042 Dellimore, K. H., Cloete, G., & Scheffer, C. (2011). Towards optimum chest
compression performance during constant peak displacement cardiopulmonary resuscitation. Medical & biological engineering & computing, 49(9), 1057-1065. doi:10.1007/s11517-011-0812-5
Delvaux, A. B., Trombley, M. T., Rivet, C. J., Dykla, J. J., Jensen, D., Smith, M. R., & Gilbert, R. J. (2009). Design and development of a cardiopulmonary resuscitation mattress. J Intensive Care Med, 24(3), 195-199. doi:10.1177/0885066609332805
Fabozzi, F. J., Focardi, S. M., Rachev, S. T., & Arshanapalli, B. G. (2014). The Basics of Financial Econometrics: Tools, Concepts, and Asset Management Applications. New Jersey: John Wiley & Sons.
43 Fischer, E. J., Mayrand, K., & Ten Eyck, R. P. (2016). Effect of a backboard on
compression depth during cardiac arrest in the ED: a simulation study. The American journal of emergency medicine, 34(2), 274-277. doi:10.1016/j.ajem.2015.10.035
Gianotto-Oliveira, R., Gonzalez, M. M., Oliveira, G. G., Zanocelo, T. M., Munhoz, B. D., Quilici, A. P., & Timerman, S. (2010). Influence of body mass index in the quality of cardiopulmonary resuscitation. Resuscitation, 81(2). doi:10.1016/j.resuscitation.2010.09.206
Go, A. S., Mozaffarian, D., Roger, V. L., Benjamin, E. J., Berry, J. D., Borden, W. B., ... Turner, M. B. (2013). Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation, 127(1), e6-e245. doi:10.1161/CIR.0b013e31828124ad
Greif, R., Lockey, A. S., Conaghan, P., Lippert, A., De Vries, W., & Monsieurs, K. G. (2015). European Resuscitation Council Guidelines for Resuscitation 2015: Section 10. Education and implementation of resuscitation. Resuscitation, 95, 288-301. doi:10.1016/j.resuscitation.2015.07.032 Handley, A. J. (2012). In-hospital chest compressions--the patient on a bed.
Resuscitation, 83(7), 795-796. doi:10.1016/j.resuscitation.2012.03.019 Hasegawa, T., Okane, R., Ichikawa, Y., Inukai, S., & Saito, S. (2020). Effect of
chest compression with kneeling on the bed in clinical situations. Japan journal of nursing science : JJNS, 17(2), e12314. doi:10.1111/jjns.12314 Hosmer, D. W., Lemeshow, S., & Sturdivant, R. X. (2013). Applied Logistic
Regression, 3rd Edition. New Jersey: John Wiley & Sons.
International Liaison Committee on Resuscitation ILCOR. (2020). Firm Surface for CPR (BLS): Systematic Review. Retrieved from
https://costr.ilcor.org/document/firm-surface-for-cpr-tfsr-costr
Jaafar, A., Abdulwahab, M., & Al-Hashemi, E. (2015). Influence of Rescuers' Gender and Body Mass Index on Cardiopulmonary Resuscitation according to the American Heart Association 2010 Resuscitation Guidelines. International scholarly research notices, 2015, 246398. doi:10.1155/2015/246398
44 Jang, J., Park, T., Lee, D., Lee, S., Kim, S., & Kim, C. (2009). Comparison of
Chest Compression Quality Between the Floor and the Bed Using Backboard. Annals of Emergency Medicine, 54(3), S139-S139. doi:10.1016/j.annemergmed.2009.06.481
Jäntti, H., Silfvast, T., Turpeinen, A., Kiviniemi, V., & Uusaro, A. (2009). Quality of cardiopulmonary resuscitation on manikins: on the floor and in the bed. Acta Anaesthesiol Scand, 53(9), 1131-1137. doi:10.1111/j.1399-6576.2009.01966.x
Kaminska, H., Wieczorek, W., Matusik, P., Czyzewski, L., Ladny, J. R., Smereka, J., ... Szarpak, L. (2018). Factors influencing high-quality chest compressions during cardiopulmonary resuscitation scenario, according to 2015 American Heart Association Guidelines. Kardiologia polska, 76(3), 642-647. doi:10.5603/KP.a2018.0003
Kleinman, M. E., Brennan, E. E., Goldberger, Z. D., Swor, R. A., Terry, M., Bobrow, B. J., ... Rea, T. (2015). Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 132(18 Suppl 2), S414-435. doi:10.1161/CIR.0000000000000259
Klickovic, A., Raffay, V., Tanasijevic, J., Atanaskovic, O., Racic, S., & Fiser, Z. (2012). BMI effect on chest compressions. Resuscitation, 83. doi:10.1016/j.resuscitation.2012.08.116
Krikscionaitiene, A., Stasaitis, K., Dambrauskiene, M., Dambrauskas, Z., Vaitkaitiene, E., Dobozinskas, P., & Vaitkaitis, D. (2013). Can lightweight rescuers adequately perform CPR according to 2010 resuscitation guideline requirements? Emerg Med J, 30(2), 159-160. doi:10.1136/emermed-2011-200634
Lin, Y., Wan, B., Belanger, C., Hecker, K., Gilfoyle, E., Davidson, J., & Cheng, A. (2017). Reducing the impact of intensive care unit mattress compressibility during CPR: a simulation-based study. Advances in simulation, 2, 22. doi:10.1186/s41077-017-0057-y
45 Monsieurs, K. G., Nolan, J. P., Bossaert, L. L., Greif, R., Maconochie, I. K.,
Nikolaou, N. I., ... Zideman, D.A. (2015). European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation, 95, 1-80. doi:10.1016/j.resuscitation.2015.07.038
Morrison, L. J., Neumar, R. W., Zimmerman, J. L., Link, M. S., Newby, L. K., McMullan, P. W., Jr., ... Edelson, D.P. (2013). Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation, 127(14), 1538-1563. doi:10.1161/CIR.0b013e31828b2770
Mpotos, N. (2013). Achievement and Maintenance of High Quality Resuscitation Skills. PhD Thesis, Ghent University, Belgium, p99 (ISBN 9789090279602)
Mpotos, N., De Wever, B., Cleymans, N., Raemaekers, J., Valcke, M., & Monsieurs, K. G. (2013). Efficiency of short individualised CPR self-learning sessions with automated assessment and feedback. Resuscitation, 84(9), 1267-1273. doi:10.1016/j.resuscitation.2013.02.020 Mpotos, N., De Wever, B., Valcke, M., & Monsieurs, K. G. (2012). Assessing basic life support skills without an instructor: is it possible? BMC Medical Education, 12(58).
Mpotos, N., Decaluwe, K., Van Belleghem, V., Cleymans, N., Raemaekers, J., Derese, A., ... Monsieurs, K. G. (2015). Automated testing combined with automated retraining to improve CPR skill level in emergency nurses. Nurse education in practice, 15(3), 212-217. doi:10.1016/j.nepr.2014.11.012
Mygind-Klausen, T., Jaeger, A., Hansen, C., Aagaard, R., Krogh, L. Q., Nebsbjerg, M. A., ... Løfgren, B. (2018). In a bed or on the floor? - The effect of realistic hospital resuscitation training: A randomised controlled trial. The American journal of emergency medicine, 36(7), 1236-1241. doi:10.1016/j.ajem.2017.12.029
Nishisaki, A., Maltese, M. R., Niles, D. E., Sutton, R. M., Urbano, J., Berg, R. A., & Nadkarni, V. M. (2012). Backboards are important when chest
46 compressions are provided on a soft mattress. Resuscitation, 83(8), 1013-1020. doi:10.1016/j.resuscitation.2012.01.016
Nishisaki, A., Nysaether, J., Sutton, R., Maltese, M., Niles, D., Donoghue, A., ... Nadkarni, V. (2009). Effect of mattress deflection on CPR quality assessment for older children and adolescents. Resuscitation, 80(5), 540-545. doi:10.1016/j.resuscitation.2009.02.006
Nolan, J. P., Soar, J., Smith, G. B., Gwinnutt, C., Parrott, F., Power, S., ... Rowan, K. (2014). Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation, 85(8), 987-992. doi:10.1016/j.resuscitation.2014.04.002
Noordergraaf, G. J., Paulussen, I. W., Venema, A., van Berkom, P. F., Woerlee, P. H., Scheffer, G. J., & Noordergraaf, A. (2009). The impact of compliant surfaces on in-hospital chest compressions: effects of common mattresses and a backboard. Resuscitation, 80(5), 546-552. doi:10.1016/j.resuscitation.2009.03.023
Oh, J., Chee, Y., Song, Y., Lim, T., Kang, H., & Cho, Y. (2013a). A novel method to decrease mattress compression during CPR using a mattress compression cover and a vacuum pump. Resuscitation, 84(7), 987-991. doi:10.1016/j.resuscitation.2012.12.027
Oh, J., Kang, H., Chee, Y., Lim, T., Song, Y., Cho, Y., & Je, S. (2013b). Use of backboard and deflation improve quality of chest compression when cardiopulmonary resuscitation is performed on a typical air inflated mattress configuration. Journal of Korean medical science, 28(2), 315-319. doi:10.3346/jkms.2013.28.2.315
Oh, J., Kim, C., Kim, S., & Lee, D. (2016). Does the bed frame deflection occur along with mattress deflection during in-hospital cardiopulmonary resuscitation? An experiment using mechanical devices. Hong Kong Journal of Emergency Medicine, 23(2). doi:10.1177/102490791602300205
Oh, J., Lim, T. H., Cho, Y., Kang, H., Kim, W., Chee, Y., ... Lee, J. (2016). Training a Chest Compression of 6-7 cm Depth for High Quality Cardiopulmonary